Home | Education | Tendon Disorders | Rotator Cuff Pathology
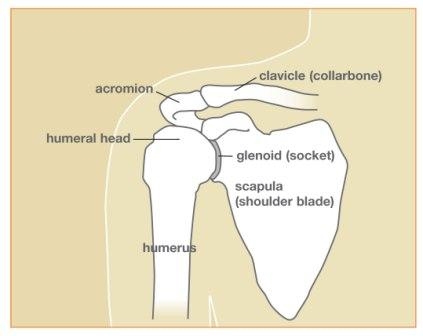
Figure 1: Shoulder anatomy
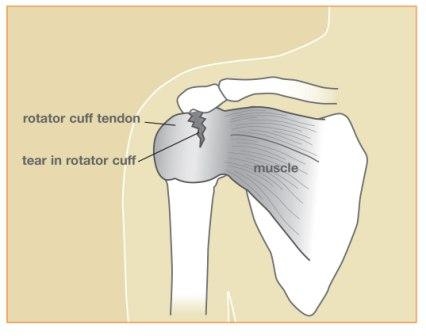
Figure 2: Rotator cuff tendon and muscles
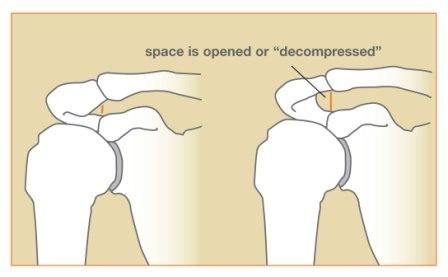
Figure 3: Pre- and post-surgery
Rotator Cuff Pathology
Rotator Cuff Pathology
The rotator cuff is the confluence of the tendons of four muscles that encompass the ball joint (humeral head) of the shoulder (see Figures 1, 2). The muscles originate on the shoulder blade (scapula) and attach (insert) on the arm bone (humerus). The rotator cuff has two functions. It provides stability to the shallow shoulder (glenohumeral) joint. Its second function is to provide motors (muscles) to move the shoulder. As time passes and we age, so does the rotator cuff. The rotator cuff tendon degenerates with age. It may also undergo wear and tear as it rubs between the acromion (tip of the shoulder blade) and the humeral head. It may become thickened and inflamed, which may be described as impingement syndrome. Changes can vary from microscopic tears and bursitis to large tears. The symptoms include pain, weakness, restricted motion, a feeling of instability, catching, and locking. Rotator cuff pathology is really a continuum or a spectrum of abnormalities ranging from a normal, asymptomatic aging process to end-stage arthritis and instability caused by absence of the rotator cuff.
Figure 1: Shoulder anatomy
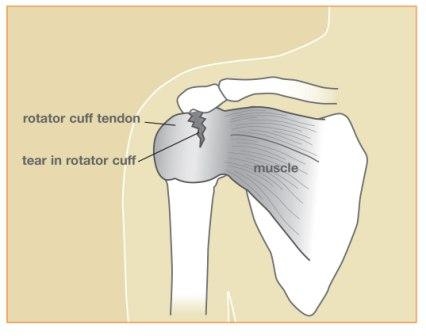
Figure 2: Rotator cuff tendon and muscles
Who gets it?
Everyone over 50 years of age has abnormalities in his or her rotator cuff. Therefore, everyone has some degree of rotator cuff pathology as he or she ages. How this pathology is manifest varies widely. Most people are not symptomatic. Onset of symptoms can be related to ordinary activities of daily living, or they can be attributed to a single event. The symptoms mentioned above are usually aggravated in certain positions, such as reaching back, for example, to fasten a seat belt or pick up a briefcase out of the back seat. Symptoms are worse when the arm is elevated overhead, higher than the shoulder, especially if the elevated arm is loaded, for example, picking up a stack of plates out of a cupboard. Overhand activities (pitching, throwing, tennis, or racquetball) commonly accentuate symptoms.How is rotator cuff pathology diagnosed?
History and physical examination are the initial evaluation that leads to diagnosis of rotator cuff pathology. Pain can be provoked by overhead maneuvers, and there may be weakness of the shoulder muscles. Plain x-rays are done to check for calcifications, arthritis, or bone problems. MRI may help to assess the tendons for inflammation and tears. Injections and arthroscopy may be used as diagnostic and therapeutic tools.What are the treatment options?
Alterations in activities and learning to use the shoulder in a safer, more comfortable manner is important. Anti-inflammatory medications are used. Physical therapy may help improve mobility and strengthen shoulder muscles. Injections are used for pain relief and their anti-inflammatory effect. Surgical intervention is usually the last option. Surgical options vary widely. Arthroscopy with limited incisions or open surgery can be done to remove inflamed bursa and impinging bone spurs, decompressing or opening up the space available for the rotator cuff (see Figure 3). The end of the clavicle (collarbone) may be removed if it has impinging spurs. Some rotator cuff tears can be repaired with arthroscopic techniques. Other tears require a larger incision and surgical exposure. Some large tears, particularly those associated with resultant arthritis, simply cannot be repaired.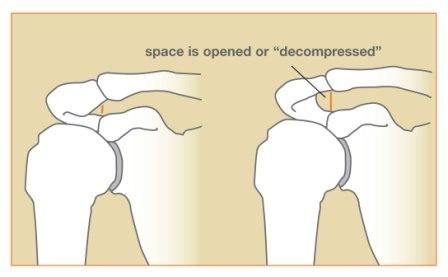
Figure 3: Pre- and post-surgery
Arthritis that occurs as a result of rotator cuff deficiency has specific characteristics and presents extraordinary challenges. When the deformity, pain, and dysfunction from the arthritis become disabling, there are major surgical options – arthroplasty (partial or total shoulder joint replacement, resection) or arthrodesis (fusion), but the expectations are more limited.
The information on this webpage is based on material from the American Society for Surgery of the Hand and is for educational purposes only.